Link
A graph of complex construction
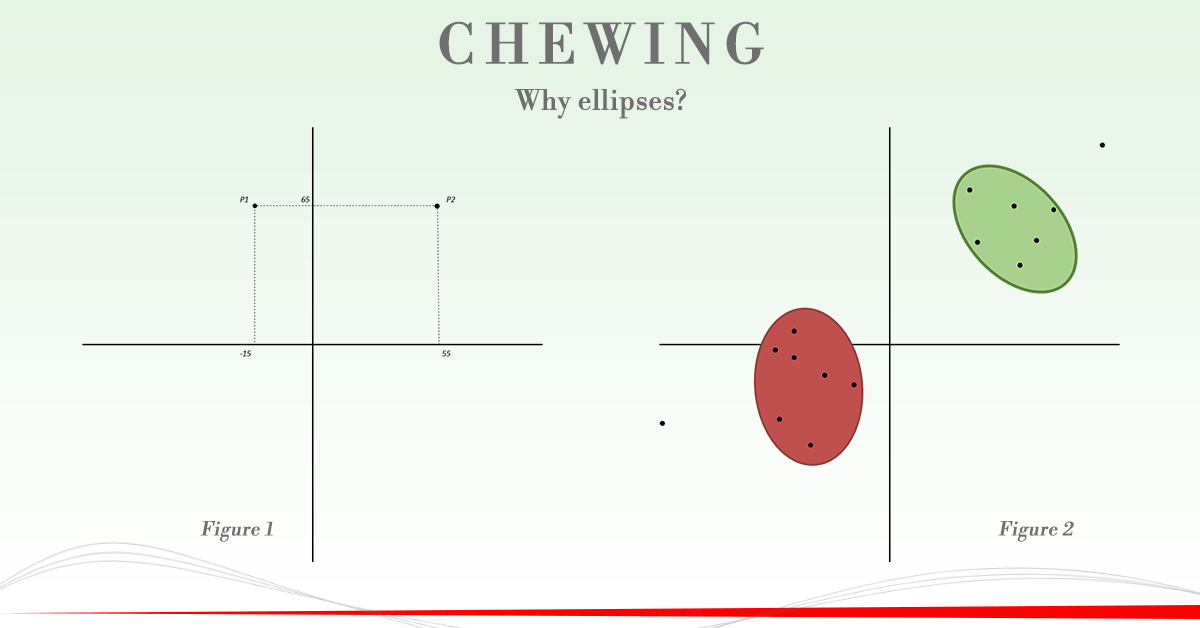
The algorithm that interprets the acquisitions concerning the dynamic chewing processes gives rise to an elliptic figure of Lissajous that is represented on a Cartesian graph. In this graph the X axis represents the differential activity of the masseters (right masseter minus left masseter) while the Y axis represents the differential activity of the anterior temporal (right anterior temporal less left anterior temporal).
Thus, during a single masticatory act, a single point is generated whose spatial coordinates X and Y will depend on the temporal-masseteric differential values specific for that act. This operation is repeated for each chewing act thus obtaining a cloud of identification points of the patient's chewing dynamics.
Then, two ellipses are generated, representing the populations of points obtained by the acquisitions of the chewing acts. One to identify those relating to chewing on the right side (green color) and one for the left side (red color). Therefore, the chewing protocol found in the ellipsis diagrams on a Cartesian plane a natural representation.
Example
The patient has chewed on the right side with the following recruitment ratios (all values refer to the standardization test carried out on the cottons):
- Right Masseter: 85% Left Masseter: 30%
- Right thunderstorm: 110% Left thunderstorm: 45%
The right-left differential for muscle pairs will therefore be:
- Masseter differentials = 85 - 30 = 55%
- Time differentials = 110 - 45 = 65%
The point identifies a single masticatory act and it will have coordinates X-Y P2 (55; 65). Having both positive coordinates will be placed in the first quadrant (top right), as in Figure 1.
Let us now consider another point, again with reference to the chewing on the right side.
- Right Masseter: 25% Left Masseter: 40%
- Right thunderstorm: 110% Left thunderstorm: 45%
In this case the right-left differential for muscle pairs will be:
- Masseter differentials = 25 - 40 = -15%
- Time differentials = 110 - 45 = 65%
The point that identifies this chewing instead will have coordinates X-Y P1 (-15; 65). This will place it in the second quadrant (top left), due to the negativity of the X coordinate, as shown in Figure 1. This example, unlike the previous one, illustrates an anomalous situation during which, although the patient is chewing on the right side, the balancing masseter (left) is more recruited with respect to the working masseter (right).
This process is carried out for all the chewing acts that follow each other during a chewing on one side. At the end of the acquisition process our chart will then be dotted with points, some belonging to the chewing on the right side and others to the one on the left side. An interpolation algorithm will take care of generating the ellipses around the points of each specific chewing, as shown in Figure 2.
Brief overview of the indices in play
In this Cartesian graph the position of the ellipses in the different quadrants does not find an anatomical correspondent in the patient. As might be mistakenly thought, the various quadrants do not in fact represent the various muscular districts (masseters below and temporal above) but are the regions of space in which the various points will be positioned.
We will not analyze if the position in which the points are found is physiologically correct or not in this article. Therefore, to understand if the ellipses are in physiologically correct positions it is useful to briefly introduce the main reference indices. To better understand the interpretation of these indices, refer to the appropriate articles on this blog:
The module is represented graphically by the distance of the center of the ellipse from the center of the Cartesian axes.
The acrophase is the angle between the straight line connecting the center of the ellipse with the center of the axes and the X axis.
The area of the ellipse indicates the area within which the center of gravity of all the chews is located and in which most of the points are collected.
A "user friendly" electromyographic approach to measuring atypical swallowing.
Link
Through the easymyo’s software and hardware technologies this interesting study was published by Friends and Colleagues Giacomo Begnoni, Maria Cadenas de Llano‐Pérula, Guy Willems, Gaia Pellegrini, Federica Musto and Claudia Dellavia. Congratulations for the interesting contribution to these standardized methods of instrumental analysis that help to better understand the mechanisms of oral physiology but also the single Patient we need to treat.
Background
Swallowing is a complex physiologic function developing mostly in the first years of life. After 6 years old, if mature deglutition is not achieved, swallowing persists as “atypical swallowing” (AS).
Objective
The aim of this study was to detect any electromyographical differences in the muscular activation pattern in patients with and without AS. Materials and methods 38 adolescents and young adults were selected for this study: 20 with atypical swallowing (AS group) and 18 without (C group). Standardised surface electromyographic analysis was performed by the same operator to detect the activity of masseter (MM), temporalis (TA) and submental (SM) muscles. A Student t test for unpaired data was carried out to detect differences between the AS and C groups. A 1‐way ANOVA was performed to detect any differences between the three couples of muscles.
Results
When compared to controls, AS patients showed a significantly longer duration of activity for each couple of muscles and for the whole duration of swallowing act (P < 0.0001) as well as lower intensity of the SM activity (P < 0.05) than controls. Within the AS and C groups, masticatory muscles (MM and TA) showed lower duration of activation (P < 0.01) and lower intensity of the spike (P < 0.0001) than SM. Within the C group, masticatory muscles also reached their activation spike earlier (1‐way ANOVA, P < 0.01) than SM.
Conclusion
Two different muscular performance models have been defined: patients with AS showed a longer activity of all the muscles involved with a lower intensity of SM activity than that of controls.
The man and the strength of the bite
Link
Title:
The craniomandibular mechanics of being human
Introduction:
Diminished bite force has been considered a defining feature of modern Homo sapiens, an interpretation inferred from the application of two-dimensional lever mechanics and the relative gracility of the human masticatory musculature and skull.This conclusion has various implications with regard to the evolution of human feeding behaviour.
Material and methods:
However, human dental anatomy suggests a capacity to withstand high loads and two-dimensional lever models greatly simplify muscle architecture, yielding less accurate results than threedimensional modelling using multiple lines of action. Here, to our knowledge, in the most comprehensive three-dimensional finite element analysis performed to date for any taxon, we ask whether the traditional view that the bite of H. sapiens is weak and the skull too gracile to sustain high bite forces is supported. We further introduce a new method for reconstructing incomplete fossil material.
Results:
Our findings show that the human masticatory apparatus is highly efficient, capable of producing a relatively powerful bite using low muscle forces. Thus, relative to other members of the superfamily Hominoidea, humans can achieve relatively high bite forces, while overall stresses are reduced.
Conclusions:
Our findings resolve apparently discordant lines of evidence, i.e. the presence of teeth well adapted to sustain high loads within a light weight cranium and mandible.
Practical tip:
We do not have to underestimate the ability to produce strength in our patients, even apparently fragile. Masticatory biomechanics is able to profit the muscle strength generating important pressures.
Fast expansion of the palate and muscular performance
Link
Title:
Longitudinal effects of rapid maxillary expansion on masticatory muscles activity
Background:
To investigate the modifications induced by rapid maxillary expansion (RME) on the electromyographic (EMG) activities of the anterior temporal and superficial masseter muscles, in patients without pre-treatment EMG alterations.
Material and Methods:
Twenty-one patients with unilateral posterior cross-bite selected from the orthodontic department of the University of L’Aquila (Italy), were enrolled. There was no control group in this study since each subject acted as a control of her/himself. Two surface EMG recordings were taken: T0 (before RME) and at T1 (3 month after the end of expansion). To verify the neuromuscular equilibrium, the EMG activities of both right and left masseter and anterior temporal muscles were recorded during a test of maximum clench. EMG indexes were compared by paired Student’s t-test.
Results:
In both occasions, all indices showed a good symmetry between the right and left side masticatory muscles. No statistically significant differences were found between the two recordings.
Conclusions:
In children without pre-treatment EMG alterations, no variations in standardized muscular activity after RME were found. The treatment did not alter the equilibrium of the masseter and temporal muscles.
Practical tip:
With a good functional management also important changes in dental occlusion can be executed maintaining the balance of the masticatory muscles.
Can orthodontic therapies that alter occlusion respect the neuromuscular balance of patients?
Link
Title:
Effects of the functional orthopaedic therapy on masticatory muscles activity
Background:
The purpose of this study was to examine surface electromyographic (sEMG) activity of masticatory muscles before and after functional orthopaedic therapy with Sander appliance.
Material and Methods:
Ten adolescents (5 girls, 5 boys) with an Angle Class II, division I malocclusion, 9-13 years old, were submitted to sEMG before and after functional orthopaedic therapy. To verify the neuromuscular equilibrium, the standardized EMG activities of right and left masseter and anterior temporal muscles were recorded during maximum voluntary clench, and analysed calculating: POC (index of the symmetric distribution of the muscular activity determined by the occlusion); TC (index of presence of mandibular torque) and Ac (index suggesting the position of occlusal barycentre). The total muscular activity was also calculated. Pre- and post- functional therapy data were compared with Wilcoxon Signed-Rank Test.
Results:
Before treatment, all subjects had a good neuromuscular equilibrium, which was not altered by treatment.
Conclusions:
sEMG evaluations allow to quantify the impact of occlusion on masticatory muscle activity and to control that the functional orthopaedic therapy maintain a good muscular coordination.
Practical tip:
Even in orthodontic therapies that alter occlusion, it is possible to respect the neuromuscular balance of patients.
Different occlusions but same muscle function! What if we consider the opposite?
Link
In this article published by friends: Francesca Vozzi, Lorenzo Favero, Redento Peretta, Luca Guarda-Nardini, Francesco Cocilovo and Daniele Manfredini (Clin Exp Dent Res. 2018 Nov 28;4(6):263-267) it’s scientifically demonstrated that, at different morphologically occlusions, do not systematically fix a different functional meaning! We could add that the opposite can be also true; at the same occlusal morphology can correspond different muscle functions. In this perspective the great majority of scientific studies on this matter, based on the research of the statistical correlations between occlusal morphology and clinical symptoms/signs, in the future could be revisited.
Title:
Indexes of jaw muscle function in asymptomatic individuals with different occlusal features.
Target:
This study aims to assess the correlation between indexes of jaw muscle function and dento-skeletal morphology.
Materials and methods:
A sample of 35 temporomandibular disorders-free healthy individuals (10 males, mean age 26.7 ± 9.8 years) underwent surface electromyographic (sEMG) assessment of bilateral masseter and temporalis muscles, to evaluate sEMG activity during maximum voluntary clenching (MVC) with a dedicated device (Easymyo®, T.F.R. Technology, Udine, Italy). Four outcome parameters were assessed for each individual: MCV on cotton rolls; MVC on teeth; chewing on right and left sides; clench/relax test. Electromyographic recordings were assessed based on five standardized indexes of muscle function, to evaluate the degree of muscle asymmetry during static and dynamic function (i.e., percentage overlapping coefficient [POC], Impact, Asymmetry, Activation, and Torque). For each individual, the presence of a number of occlusal and skeletal features was assessed: asymmetry of molar class; deviated incisor midline; deep bite; open bite; and crossbite. Skeletal class and vertical dimension of occlusion were also evaluated. Based on normality distribution of data, t test and analysis of variance, when needed, were used to compare muscle function indexes between individuals with and without the different dento-skeletal features.
Results:
None of the musclefunction indexes (POC, Impact, Asymmetry, Activation, and Torque) was significantly different between individuals with or without the various dental and skeletal features. Gender differences were also not significant (p > 0.05). Despite some minor differences were observed, none of them was significant.
Conclusion:
Thus, the interaction between form and function is too complex for hypothesizing a simple one-to-one relationship between interarch tooth relationship and muscle function patterns.
Practical tip:
Not consider a specific morphology as assurance of presence or absence of specific motor models.
Occlusal Morphology 1 Year after Orthodontic and Surgical-Orthodontic Therapy / A Quantitative Analysis of Clinically Successful Patients
Link
Title:
Morphology of the occlusion after a year from orthodontic and surgical-orthodontic therapy
Quantitative analysis on patients with a positive clinical response
Target:
The study evaluated the morphological characteristics of the occlusion in patients with a positive clinical response following orthodontic treatment or orthodontic surgery. In particular, points, areas and frequency of occlusal contact were evaluated after a year of passive retention.
Materials and methods:
Two groups of patients were analyzed: twenty-two orthodontics and eighteen surgical-orthodontics.
All patients were treated with edgewise technique by the same orthodontist.
Points and contact areas were evaluated using a new digital image analysis method considering the occlusal impression. The polyvinylsiloxane impressions, after being detected, were scanned and transformed into grayscale images.
The physical relationship of light absorbance, between the polyvinylsiloxane and a known thickness, has served to determine the contact areas (less than 50 μm in thickness) and those in close contact (less than 350 μm in thickness).
Results:
The contact area was significantly larger in orthodontic patients than in orthodontic surgery cases (Student's t-test, P.05). The surgical-orthodontic group had significantly fewer contact points than the orthodontic group only at 150 μm of thickness.
In both groups of patients the first molar had the largest contact surface and that the occlusal support was mainly distributed in the posterior regions with predominance of the first molar.
Conclusion:
Surgical-orthodontic patients appear to have smaller contact surfaces and fewer contact points than orthodontic patients do. However, there are no differences in the number of teeth in contact with the opposing teeth.
Practical tip:
The contact symmetry of the first molars is probably a key factor in the post-orthodontic normalization of the contact points.
Patients with vestibular lesions: is it useful to include a neck muscles analysis?
Link
Title:
Electromyographic activity of sternocleidomastoid and masticatory muscles in patients with vestibular lesions
Objectives:
This study evaluated the electromyographic characteristics of masticatory and neck muscles in subjects with vestibular lesions.
Material and methods:
Surface electromyography of the masseter, temporalis and sternocleidomastoid muscles was performed in 19 patients with Ménière’s disease, 12 patients with an acute peripheral vestibular lesion, and 19 control subjects matched for sex and age.
Results:
During maximum voluntary clenching, patients with peripheral vestibular lesions had the highest co-contraction of the sternocleidomastoid muscle, the control subjects had the smallest values, and the patients with Ménière’s disease had intermediate values. The control subjects had larger standardized muscle activities than the other patient groups.
Conclusion:
In conclusion, during maximum voluntary tooth clenching, patients with vestibular alterations have both more active neck muscles, and less active masticatory muscles than normal controls. Results underline the importance of a more inclusive craniocervical assessment of patients with vestibular lesions.
Practical tip:
The analysis of the involvement of the sternocleidomastoid muscles occurs during a 6-channel examination and provides for the introduction of a further measure of normalization of the activity of the sternocleidomastoid muscles. Specifically, it is necessary to explain to the patient that he will be asked to slowly rotate his head first to the right and then to the left in a period of 15 seconds. When performing this movement, make sure that the shoulders are held firm by the patient so that they do not rotate together with the neck. This allows the muscle to perform maximum contraction (maximum contralateral torsion). Subsequently the usual operations foreseen by the protocol of maximum contraction (tightening on the cotton rollers and on own teeth) are carried out.
Occlusion, neck muscles and balance: possible functional couplings?
Link
Title:
Occlusion, Sternocleidomastoid Muscle Activity, and Body Sway: A Pilot Study in Male Astronauts
Objectives:
The modifications induced by microgravity on the coordinated patterns of movement of the head, trunk, and limbs are reported on extensively. However, apparently, there is little data on the masticatory muscles. In normal gravitational conditions, information from the neck and stomatognathic apparatus play a role in maintaining the body’s balance and equilibrium. The current pilot study used normal gravity conditions to investigate the hypothesis of a functional coupling between occlusion and neck muscles and body postural oscillations.
Material and methods:
The immediate effect of modified occlusal surfaces on the contraction pattern of the sternocleidomastoid muscles during maximum voluntary clenching and on the oscillation of the center of foot pressure was analyzed in 11 male astronauts (aged 31-54 yrs). All subjects were healthy and free from pathologies of the neck and stomatognathic apparatus. Occlusal splints were prepared using impressions of their dental arches. The splints were modeled on the mandibular arch, had only posterior contacts, and were modified to obtain a more symmetric, standardized contraction of the masseter and temporalis muscles during teeth clenching. Surface EMG activity of the sternocleidomastoid muscles was recorded during a maximal voluntary clench with and without the splint. Sternocleidomastoid potentials were standardized as percent of the mean potentials recorded during a maximum contralateral rotation of the head, and the symmetry of the EMG waves of left- and right-side muscles was measured. Body sway was assessed with and without the splint, either with eyes open or closed. The variations of the center of foot pressure were analyzed through bivariate analysis, and the area of the 90% standard ellipse was computed. Within each visual condition (eyes open or closed), the difference between the areas of oscillation measured with and without the splint was computed.
Results:
Muscular activity was more symmetric with the splint. The area of oscillation of the center of foot pressure was larger without the splint than with the splint, both with eyes open and eyes closed. The modifications, induced by the occlusal splint in the sternocleidomastoid muscles’ symmetry, and center of foot pressure differential area with closed eyes, were significantly related (p<0.05): the larger the increment in muscular symmetry, the smaller the area of oscillation with the splint as compared to without the splint.
Conclusion:
A functionally more symmetric maxillo-mandibular position resulted in a more symmetric sternocleidomastoid muscle contraction pattern and less body sway. Modifications in the contraction of the masticatory muscles may therefore affect the whole body.
Practical tip
The analysis of the involvement of the sternocleidomastoid muscles occurs during a 6-channel examination and provides for the introduction of a further measure of normalization of the activity of the sternocleidomastoid muscles. Specifically, it is necessary to explain to the patient that he will be asked to slowly rotate his head first to the right and then to the left in a period of 15 seconds. When performing this movement, make sure that the shoulders are held firm by the patient so that they do not rotate together with the neck. This allows the muscle to perform maximum contraction (maximum contralateral torsion). Subsequently the usual operations foreseen by the protocol of maximum contraction (tightening on the cotton rollers and on own teeth) are carried out.
Electromyographic evaluation of implant-supported prostheses in hemimandibulectomy-reconstructed patients
Link
Title:
Electromyographic evaluation of implant-supported prostheses in hemimandibulectomy-reconstructed patients
Objectives:
To assess the clinical conditions, patient’s satisfaction and functional outcomes in oral neoplasia patients with hemimandibulectomy, bone reconstruction and implant- supported prosthesis.
Material and methods:
Twelve patients after mandibular resection (with and without condyle), reconstruction and successful fixed implant-supported prosthesis rehabilitation were examined. Patients underwent clinical evaluation and filled in a questionnaire about their satisfaction toward oral functions. Surface electromyography (EMG) of the masticatory muscles was performed during a 15-s unilateral gum chewing test. EMG potentials were standardized as percentage of a maximum clench on cotton rolls and compared with reference data obtained from 20 healthy subjects.
Results:
Excellent clinical and radiological parameters were found. Patients stated a decreased post-rehabilitation satisfaction toward mastication and phonetics, but an increased attention to oral care. Only patients with condylar resection reported augmented esthetic scores. In both the resected and the remaining sides, chewing frequency was higher in the patients than in the reference group. Pooled muscle activities (sum of the integrated areas of the EMG potentials over time) were larger in patients than in control subjects, particularly in the non-operated side. The percentage contribution of working-side muscular activity in the operated side was similar to reference values, but significantly inferior in the opposite side. The patterns of muscle contraction during unilateral chewing were more variable in the reconstructed patients than in control subjects; the difference was significant only in the non-operated side.
Conclusion:
Post-rehabilitation median scores of the questionnaire indicated a positive judgment of the treatment. EMG analysis showed that functional recovery in hemimandibulectomy patients was satisfactory, although some alterations were observed in the non-operated side of mastication.
Practical tip
The analysis of the involvement of the masticatory muscles in a dynamic chewing act occurs during a 4-channel examination and provides for the introduction of two one-sided chewing tests after the maximum voluntary contraction examination on the cotton rolls. Specifically, it is necessary to explain to the patient that he will be asked to chew a chwingum (a bolus that is not consumed over time) on one side of the mouth for a period of 15 seconds, and then on the opposite side for 15 seconds too. When performing this movement, make sure that the patient is kept upright and the shoulders still.
Evidence of an influence of asymmetrical occlusal interferences on the activity of the sternocleidomastoid muscle
Link
Title
Evidence of an influence of asymmetrical occlusal interferences on the activity of the sternocleidomastoid muscle.
Introduction and purpose
Verify the hypothesis that there is a functional coupling between occlusion and neck muscles. This aim was achieved through the use of asymmetric occlusal interferences to evaluate how and how much the contraction activity of the sternocleidomastoid muscles was modified during an act of maximum voluntary clench.
Materials and methods
Surface electromyographic examinations, according to the method established by the protocol in use at the laboratory, were performed on 30 healthy subjects whose symmetric activity of the contraction muscles of masseter muscles, anterior temporalis and sternocleidomastoid muscles was first evaluated during a maximum voluntary contraction. Subsequently, occlusal interferences of 200μm were introduced on teeth 16, 13, 23 and 26 and the electromyographic tests were re-performed with maximum contraction.
Results
In all the tests of maximum contraction without interference, a mean POC greater than 87% was recorded for all subjects, identifying a symmetric activity of muscular activation. The alteration of the occlusal surface instead showed a highly variable POC and a substantial asymmetry of the recruitment pattern of the sternocleidomastoid muscles.
Conclusions
The work has therefore highlighted that in the presence of a malocclusion not only there are changes to the patterns of recruitment of the masticatory muscles, as previously demonstrated, but also a change in the recruitment activities of the neck muscles. The identification of functional couplings between the stomatognathic and the locomotor systems of the neck suggests that particular attention should be paid, for example, to the occlusion of patients suffering from cervical problems. Finally, the lack of a relationship between the localization of occlusal interference and the recruitment asymmetry suggests the presence of complex and highly subject dependent mechanisms of regulation and compensation.
Practical tip
The analysis of the involvement of the sternocleidomastoid muscles occurs during a 6-channel examination and provides for the introduction of a further measure of normalization of the activity of the sternocleidomastoid muscles. Specifically, it is necessary to explain to the patient that he will be asked to slowly rotate his head first to the right and then to the left in a period of 15 seconds. When performing this movement, make sure that the shoulders are held firm by the patient so that they do not rotate together with the neck. This allows the muscle to perform maximum contraction (maximum contralateral torsion). Subsequently the usual operations foreseen by the protocol of maximum contraction (tightening on the cotton rollers and on own teeth) are carried out.
MODULUS: how much does the balancing side have to work to protect the joints during chewing?
Link
MODULUS: how much does the balancing side have to work to protect the joints during chewing?
Definition
The modulus is represented graphically by the distance of the center of the ellipse from the center of the Cartesian axes (red and green lines). This means that the greater this value is (and therefore the more far from the center the ellipse is located) the greater is the differential between the two pairs of muscles during a chewing test on one side. It helps to understand if chewing involves more the working antimer than the balancing one.
In normal situations it has an average value of 90.
Example
Consider the graphs in Figure 1 and Figure 2, where the ellipses are positioned within the quadrants in which they are expected to be in normal conditions.
We can see that the ellipse on the right chewing (green) is found in both graphs in the first quadrant: in a case very far from the center, in the other very close.
In accordance with what is said in the article "Beware of chewing!", already available in this blog, the right-left muscle activation differential for the two pairs of muscles (green line) is, in both configurations, in favor of the entire right antimer (right masseter> left masseter, right anterior temporal> left anterior temporal).
In the first case, however, the module is very high (elongated line) while in the second it is very low (short line):
These two graphs, apparently analogous for the positioning of the ellipses, describe two different situations regarding the right chewing: one in which the patient has developed a strong differentiation of muscle recruitment between the two antimers and one in which there is no specific pattern of recruitment.
For completeness of analysis instead the left chewed (red) is located at the bottom left in the third quadrant in both examples. Also in this case the left-right muscle activation differential for the two pairs of muscles is very high (elongated red line) and also in this case the working side has worked more than the balancing side
Conclusions
These examples make us understand that the value of the modulus is therefore an index of how much high or low the muscular activation differential of the two muscle pairs is (balancing side vs. working side) but does not provide indications on where the balance is between the 4 muscles investigated during dynamic chewing. In fact, we may have cases in which the ellipses are not positioned in a physiologically correct way (quadrants different from those expected under normal conditions). For this reason it is necessary to integrate also the Acrofase index during the interpretation of this graph, to understand if the positioning of the ellipses respects what we would expect in normal conditions.
Mandibular molar reconstruction altering habitual occlusion
Link
Through this treatment we analyze an example of how the surface electromyography analysis can be integrated into the steps that lead to the reconstruction of a mandibular molar, helping the Professional to have an instrumental measurement of the alterations that he is performing in the patient's mouth.
Link under the image
Beware of chewing!
Link
A graph of complex construction
The algorithm that interprets the acquisitions concerning the dynamic chewing processes gives rise to an elliptic figure of Lissajous that is represented on a Cartesian graph. In this graph the X axis represents the differential activity of the masseters (right masseter minus left masseter) while the Y axis represents the differential activity of the anterior temporal (right anterior temporal less left anterior temporal).
Thus, during a single masticatory act, a single point is generated whose spatial coordinates X and Y will depend on the temporal-masseteric differential values specific for that act. This operation is repeated for each chewing act thus obtaining a cloud of identification points of the patient's chewing dynamics.
Then, two ellipses are generated, representing the populations of points obtained by the acquisitions of the chewing acts. One to identify those relating to chewing on the right side (green color) and one for the left side (red color). Therefore, the chewing protocol found in the ellipsis diagrams on a Cartesian plane a natural representation.
Example
The patient has chewed on the right side with the following recruitment ratios (all values refer to the standardization test carried out on the cottons):
The right-left differential for muscle pairs will therefore be:
The point identifies a single masticatory act and it will have coordinates X-Y P2 (55; 65). Having both positive coordinates will be placed in the first quadrant (top right), as in Figure 1.
Let us now consider another point, again with reference to the chewing on the right side.
In this case the right-left differential for muscle pairs will be:
The point that identifies this chewing instead will have coordinates X-Y P1 (-15; 65). This will place it in the second quadrant (top left), due to the negativity of the X coordinate, as shown in Figure 1. This example, unlike the previous one, illustrates an anomalous situation during which, although the patient is chewing on the right side, the balancing masseter (left) is more recruited with respect to the working masseter (right).
This process is carried out for all the chewing acts that follow each other during a chewing on one side. At the end of the acquisition process our chart will then be dotted with points, some belonging to the chewing on the right side and others to the one on the left side. An interpolation algorithm will take care of generating the ellipses around the points of each specific chewing, as shown in Figure 2.
Brief overview of the indices in play
In this Cartesian graph the position of the ellipses in the different quadrants does not find an anatomical correspondent in the patient. As might be mistakenly thought, the various quadrants do not in fact represent the various muscular districts (masseters below and temporal above) but are the regions of space in which the various points will be positioned.
We will not analyze if the position in which the points are found is physiologically correct or not in this article. Therefore, to understand if the ellipses are in physiologically correct positions it is useful to briefly introduce the main reference indices. To better understand the interpretation of these indices, refer to the appropriate articles on this blog:
The module is represented graphically by the distance of the center of the ellipse from the center of the Cartesian axes.
The acrophase is the angle between the straight line connecting the center of the ellipse with the center of the axes and the X axis.
The area of the ellipse indicates the area within which the center of gravity of all the chews is located and in which most of the points are collected.
Looking for the right direction
Link
Definition
The Compass function is an additional function that helps locate the areas from which the alteration of muscular work most likely originates on the dental arch. By clicking on the appropriate button it will show a graph consisting of black lines superimposed on the image of a dental arch.
The upper lines are directed at the molars and those below the premolars. The more a line is covered by the graph (green, yellow, or red) the more the "work" of that muscle in that area of the mouth is altered in its performance.
There are two factors to consider for the correct interpretation of the chart:
Form
More the vertices will be positioned near the ends of the black lines the more we will be far from a physiological situation (both in excess and in defect), indicating that there is an imbalance in muscle recruitment.
Also, the shape is important: a very narrow and elongated shape towards a specific area of the mouth will indicate that a muscle is definitely more altered than others (as in figure 2, 4 and 6), a form wider and more symmetrical it will indicate a generalized imbalance, and therefore with less specific indications of work (as in figures 1, 3 and 5).
Color
The area and the shape of the quadrilateral give information on the location of the problem, but not on the severity of the imbalance. The latter is highlighted by a color code, depending on how much the muscular work performed is far from the physiological "normal" conditions.
In particular, the color of the directional graph depends on the value farthest from normality (both in excess and in defect) that is recorded among those of all the muscles analyzed.
Three situations can be identified:
A situation similar to Figure 1 is therefore desirable, as opposed to Figure 6, although the latter has a much smaller area and shape.
Figure 1
The temporal muscles and the right masseter have slightly altered performances (green graph therefore relatively modified values); the left masseter, on the other hand, has optimal performance values (the black line leading to the left molar areas is not covered by the green graph). The compass suggests changing the occlusal dimensions of the entire arch except the left molar area.
Figure 2
Example opposite to that visible in Figure 1; always in contexts very close to normality, the only line covered by the graph (witnessing alteration of the muscle that exerts forces in that area) is that which directs itself in the left molar area. In this condition the compass function initially suggests trying to modify the occlusal support in the left molar area. All the rest of the arch seems to be a correct three-dimensional dimension.
Figure 3
In this example all the muscles are altered in their performance significantly. It is advisable to alter the vertical dimension in the whole dental arch, also altering its three-dimensionality.
Figure 4
In this condition an important alteration of the left masseter function is shown suggesting a different support in the left molar area. Probably an alteration of three-dimensionality will be necessary.
Figure 5 and 6
They represent conditions during which serious alterations in muscular performance occurred respectively for all the muscles investigated (Figure 5) and for the right masseter (Figure 6). We recommend that you repeat the exam.
IMPACT: to understand if and how much the muscles are inhibited
Link
Definition
IMPACT represents the ratio of the intensity of muscular work performed during a test compared to that performed during a normalization test. The IMPACT index is influenced by occlusal stability because there is a relationship between muscle activity and number of occlusal contacts.
Muscle activity is therefore influenced by the number, the distribution and the area of occlusal contacts. It can suggest if the patient is a habitual latcher (development of parafunctions, serration, grinding) or activates proprioceptive inhibition mechanisms.
Example aspects
Healthy subjects are able to express from 80 to 120% of the activity performed on the cottons. Minor values indicate a proprioceptive inhibition attributable to dental contact.
TORQUE: avoiding undesired torsions in the long run
Link
Definition
The TORQUE torsion index measures the differential activity of the right temporal and of the left masseter in relation to the antagonist pair. As a consequence, it can be used as a potential indicator of lateral displacement forces, which in the long run, if underestimated, can influence the rehabilitative treatments that are performed on the Patient.
Example aspects
A prevalence of the right temporal and left masseter muscles can result in twisting forces on the mandible with latero-deviation to the right; in this case the torsion index will be positive.
A dominance of the left temporal and right masseter muscles will be visualized by a negative TORQUE index, indicating twisting forces to the left.
95% of healthy subjects show TORQUE values between + 10% and -10%.
Safer condyles thanks to the asymmetry index
Link
Definition
It compares the influence of dental contact on the total activity of the right antimere to the left one. This value indicates how much the right muscles are influenced by the dental contact compared to the left ones and helps to identify if there is an eventual asymmetry in the distribution of the occlusal contacts. In the presence of strong asymmetries, the condylar loads may be strongly unbalanced with a higher probability of introducing temporo-mandibular disturbances.
Example aspects
A positive index shows a prevalence of activity of the right muscles. A negative index indicates, instead, a greater differential activity of the left antimere. 95% of healthy subjects have asymmetry values between + 10% and -10% (0% no asymmetry).
The activation index: suggestions on the position of the center of gravity?
Link
Definition
The activation index compares the influence of dental contact on the activity of thunderstorms in relation to that of masseter. The activation index evaluates the prevalence of contacts on the sagittal plane, the relative position of the occlusal centre of gravity and the mandibular lever arm, when the dental arches are in contact. It is within a range of-100% to + 100%, calculated on the average maximum contraction value, compared to the value zero (0) instead of 100%.
Examples
A negative index may involve a greater differential recruitment of the temporal muscles (anterior center of gravity) or a relative inhibition of the masseter muscles, as shown in the left figure of the image. For example, in the absence of one or more molars, the masseter could be inhibited in their maximal performance to avoid the overload of the temporomandibular joint structures.
A positive index indicates a prevalence of the masseter muscles (posterior center of gravity), as shown in the right figure. 95% of healthy subjects have activation values ranging from + 10% to-10%.
What is poc?
Link
Definition
The Percentage Overlapping Coefficient (POC) indicates, in percentage, how similar it is not only in terms of intensity of contraction but also in terms of activation time, the influence of dental contact on the muscles in the left antimere compared to the right one (overlap of the activation areas). It is possible to identify POC indices relative to the pair of masseters "POC MM" or anterior temporals "POC TA".
Examples
A hypothetical 100% POC identifies that the analyzed muscle pair is influenced in the same amount by the dental contact. This implies that the activation areas will be very similar in intensity and duration of contraction, as in the left image. This does not exclude that the electrical activity that the muscles have generated may be higher or lower than the standardization test.
The POC is elaborated in all the protocols available to compare the activities of masseters, temporals, sternocleidomastoids and trapezoids. 95% of healthy subjects have POC values between 80% and 90%.
In case of lower values, a situation similar to the one shown in the right-hand images may appear, in which the activation areas, although exhibiting a similar activity in terms of intensity of activation, show a low overlap due to different activation times.
Consequences
Ultimately the POC is an index of performance symmetry, it describes if the muscles we are analyzing respond in a synchronized way to the dento-periodontal influences encountered during a maximal intercuspidal exercise.
Additional advantages of normalization
Link
Break down the influence of errors
The normalization of the electromyographic measurement not only allows to understand how much a muscle is involved with respect to its maximum capacity of contraction (see the article WHAT MEANS TO NORMALIZE within this blog) but also allows to improve the repeatability of the measures.
To better understand this further advantage, some concepts must be defined:
In light of this it is clear that a standardization procedure certainly does not eliminate errors that may alter the measurements made, but allows to minimize their influence in terms of evaluation of the results obtained. Any errors present would affect the reference values in the same way as the test values, thus making the normalized values devoid of these influences.
Example
In the above example we assume the hypothesis that between the two contraction exercises (Case 1 and Case 2) to change is only one variable, that is the positioning of the right electrodes.
As shown in the image, the electromyographic traces of the reference measurements (Figure 1.1 and 2.1) and of the test measurements (Figures 1.2 and 2.2) are different. This is because by changing the position of the electrodes, with the same muscular contractile capacity, and therefore with the same intrinsic electrical activity generated, the electrical activity actually detected by the electrodes placed on the skin has changed.
In pie charts superimposed on the previously mentioned electromyographic paths, this is even more evident. The positioning of the electrodes has changed the recruitment ratios detected during the acquisitions, influencing both the reference measure and the measure of tests that we remember, both are pure measures and therefore subject to changes due to biological and technical variables, in this specific case the position of the electrodes. Over time, however, the amount of adipose tissue, the soft tissue impedance, the contractile capacity of the muscles, etc. can also change.
However, observing Figures 1.3 and 2.3 (the normalized test measurements) it is clear that the reference measurement and the test measurement have been influenced in the same way by the different positioning of the electrodes, the normalized test is very similar in Cases 1 and 2.
Introduction of a comparative analysis method
In conclusion, the normalization of the electromyographic measurement allows:
Working with reliable control criteria, it is possible to modify only one of the variables that we know how to influence the measurements we make, identifying, thanks to the normalized measures, its real impact at the level of the electromyographic patterns.
What means to normalize
Link
In math
Normalizing means expressing a value as a percentage of another value considered as reference. In this way the normalized data result most comparable with each other as they are related to a common measure.
In surface electromyography
Normalizing an electromyographic measurement means detecting the electrical activity generated during the contraction of a muscle in a particular condition. Usually this condition must be highly repeatable and easy to perform such as a maximum static (isometric) contraction. Assuming the hypothesis that a muscle in maximum static contraction makes an effort equal to 100% of its ceiling, the electric activity (normalized) produced during any other exercise will indicate the necessary effort to perform the gesture under examination.
This general procedure can be applied to each individual muscular district that could be investigated by superficial electromyography, and it is possible to identify the maximal strain of each muscle by thinking of a specific test of maximum static contraction for that given muscle.
In clinical practice
When analyzing the electrical activity of several muscle groups simultaneously, the pure values of these individual measurements will be proportional to the specific contraction force of each muscle. Absolute measurements of this type do not provide information on how much each muscle has been involved compared to its maximal contraction.
Example
We want to evaluate the activity of 3 muscles during a contraction exercise and how much each muscle is involved:
Concluding then, both series of graphs provide useful information:
Ultimately, it can be stated that although the muscle highlighted by the circle, due to its specific characteristics of strength, was able to generate greater electrical activity, in reality it turned out to be the one least involved in terms of recruitment.
Preliminary approach for the surface electromyographical evaluation of the oral phase of swallowing
Link
BACKGROUND:
Swallowing is a muscular activity that occurs both after mastication and spontaneously as a result of saliva accumulation. Spontaneous saliva swallowing occurs about every 2 minutes. Comprehension of its functional mechanisms is relevant to assess their modification in clinical situations. A standardised surface electromyographical (ssEMG) protocol for the evaluation of this muscle activity is lacking.
ACHIEVMENTS:
Aims of the present study are:
METHODS:
Standardised surface electromyographical activity of MM, TA and SM during swallowing of saliva spontaneously accumulated was recorded in 20 healthy participants. Functional indexes including symmetry (POC), recruitment (Impact), duration of activation of each couple of muscles and of the whole exercise, position, intensity of the spike were computed. Inter- and intra-appointment reliabilities were assessed and method errors calculated. Descriptive statistics, sex- and muscles-related comparisons were carried out.
RESULTS:
Standardised surface electromyographical assessment of MM, TA and SM muscles was reliable. A high inter-individual variability was found. Percentage overlapping coefficient (POC) values were close to 80% for TA and SM, higher than for MM (P < .001). Impact values ranged between 16.4% and 30.7%, and differences were found between muscles (P < .001). The global muscle activity during swallowing lasted between 1.5 and 1.8 seconds. For each couple of muscles, the duration of activation ranged between 0.7 and 1.6 seconds and muscles-related differences were found (P < .001). The spike of activation for each couple of muscle ranged between 35.7% and 44.2% of the duration.
CONCLUSIONS:
The protocol was reliable and intra-participants repeatable measures can be carried out. Due to the high inter-participants variability, further analyses are needed to draw a model of muscular activity.
KEY WORDS:
submental muscles, surface electromyography, swallowing
This approach then opens up the possibility of introducing a new method of functional analysis in the daily clinic to study the phenomenon of swallowing.
The importance of normalizing the electromyographic measurement
Link
Cotton rolls pie chart
This graph shows the data related to the standardization measurement performed with the cotton rolls interposed between the two arches (with reduced dento-periodontal proprioception). It is possible to identify 4 quadrants related to 4 specific muscles according to the protocol in execution (Figure 1).
A specific muscle is associated with each color. The size of each slice is proportional to the electrical activity generated by that muscle compared to the others taken into consideration within the same graph. The relative dimensions of the cake slices are specific to each patient and are due to the muscular balances developed by that particular patient. All subsequent tests will be normalized on this measurement.
μV pie chart
This graph shows the data related to the measurement performed with the teeth in contact (or prostheses, plates, occlusal, bite, etc.) (Figure 2).
As in the Cotton rolls pie chart, a specific muscle is associated with each color and the size of the pie slice is proportional to the activity of that muscle compared to the others examined.
Percent pie chart
In this graph (Figure 3) the result of the overlapping of the Cotton rolls and μV pie charts is displayed. It expresses the standardized differential activity, attributable to dental contact.
Scientific studies have shown that young healthy subjects, without functional and morphological alterations, exercise similar muscular performances by tightening their teeth in maximum intercuspation or with cotton rolls between the arches. In this condition the percent pie chart will represent 4 equal slices. When this does not happen it means that in maximum intercuspation the subject has established a muscle recruitment different from that performed with the cotton rolls and so it is advisable to investigate the possible causes.
The normalized quantification of the dento-periodontal proprioceptive component thus extrapolated has two main advantages:
Correlation between indices of muscular function and dento-skeletal morphology: experimental clinical study
Link
Orthodontic-surgical treatment: electromyographic and kinesiographic evaluation in follow up period. Experimental study
Link
Are the bite force and electromyographic activity altered in muscle TMD patients with abfraction lesions?
Link
Objective: To verify if the maximal molar bite force (BF) and the electromyographic activity (EMG) are altered in TMD patients with abfraction lesions (AL) when compared to those without AL. Methods: The sample was composed of 45 patients (18–60 years old), 30 diagnosed with TMD (RDC/TMD) (15 with AL and 15 without AL) and 15 controls. The BF and the EMG of the masticatory muscles (maximal voluntary contraction (MVC) and chewing gum) were measured. Results: TMD patients showed decreased BF (p < 0.001), without differences between patients with and without AL. The electromyographic activity during MVC was similar among all groups (p > 0.05), although there was a greater trend of muscular balance for the control group (percentage overlapping coefficient and electromyographic indexes). The TMD group without AL showed a lower number of cycles and masticatory frequency. Discussion: TMD patients with and without AL exhibited similar results in the analysis of the BF and EMG, without differences.
Standardized EMG as occlusal analysis
Link
Standardized EMG as occlusal analysis
Two molars reconstruction modofying habitual occlusion.
Link
Two molars reconstruction modifying habitual occlusion.
What is POC index?
Link
The POC index (Percentage Overlapping Coeeficient) is a standardized index obtained processing two homologous muscles electromyographic signal.
Electromyographic assessment of jaw muscles in patients with All-on-Four fixed implant-supported prostheses
Link
This study evaluated the electro- myographic (EMG) characteristics of masticatory muscles in patients with fixed implant-supported prostheses according to All-on-Four® principles and in control healthy dentate subjects. Twenty- six subjects aged 50–74 years were examined. Eighteen were edentulous and had been successfully rehabilitated with (i) mandibular All- on-Four® implant-supported fixed prostheses and maxillary complete dentures (10 patients) and (ii) mandibular and maxillary All-on-Four® implant- supported fixed prostheses (eight patients). Eight reference subjects had natural dentition. Surface EMG recordings of the masseter and temporalis muscles were performed during maximum voluntary teeth clenching and during unilateral gum chewing. All values were standardised as percentage of a maximum clenching on cotton rolls. During clenching, a good global neuro- muscular equilibrium was found in all parti- cipants. During chewing, all groups had similar values of working-side muscle activities and of chewing frequency. No significant differences in the analysed EMG parameters were found between the patients with mandibular and maxillary All- on-Four® implant-supported prostheses and the reference subjects. In contrast, standardised pooled muscle activities and standardised muscular activities per cycle were larger in patients with a maxillary removable prosthesis than in control subjects (Kruskal–Wallis test, P < 0?01). Also, patients wearing a complete maxillary denture showed a poor neuromuscular coordination with altered muscular pattern and lower values of the index of masticatory symmetry than dentate control subjects (P < 0?01). EMG outcomes suggest that All-on-Four® implant-supported prostheses may be considered a functionally efficient treat- ment option for the rehabilitation of edentulous patients with reduced residual bone volume.
Comparing the electromyographic features of the Masseter and Temporal Muscles in patients with full mouth implant-supported FDPs and natural dentition.
Link
A simplified illustration of the biomechanical concept for the interpretation of the activation index.
Link
A simplified illustration of the biomechanical concept for the interpretation of the activation index.
A proposal to simplify the tridimensional definition of the vertical dimension of occlusion guided by standardized surface electromyography.
Link
A proposal to simplify the tridimensional definition of the vertical dimension of occlusion guided by standardized surface electromyography.
Standardized electromyographic analysis of swallowing and clinical applications.
Link
At the following link is available Dr. Federica Musto's PhD thesis, an interesting work that sets the basis for the swallowing standardized electromyographic analysis. Congratulations to Federica for the success that is a starting point for a more in-depth understanding of the complex gesture of swallowing.
Comprehensive Approach to the Treatment of Temporomandibular Disorder with Severe Pain Syndrome.
Link
of intraarticular TMJ elements and a change in the structure of the masticatory muscles was revealed. The best results were achieved in the group with injections of BTX-A into the masticatory muscles. Electromyographic indexes have approached the values of the norm. The clinical signs of TMD decreased or reduced.
Standardised surface electromyography allows effective submental muscles assessment
Link
Three Universities collaborare proving electromyograph indexes reliability
Link
This interesting scientific publication is the result of a research collaboration between the University of Milan, the North-Western State Medical University in St. Petersburg (Russia) and the Moscow State University in Moscow (Russia). The research concludes that sEMG indexes allow to evaluate occlusal-induced proprioceptive mediated muscular recruitment in a reliable way. This measurement protocol can be clinically applied to estimate the muscular adaption to new occlusal conditions or to re-establish physiological muscular coordination; a clinical application is showed.
Neck and shoulder muscle activity and posture among helicopter pilots and crew-members during military helicopter flight.
Link
Study about vertical dimension of occlusion electromygraphycally defined.
Link
In this study carried out at the Department of Oral and Maxillofacial Sciences-Prosthodontics Unit, University “Sapienza” of Rome has been evaluated the possibility to determine an individual correct vertical dimension of occlusion (VDO) through the use of surface electromyography (sEMG). A total of 20 patients that required a prosthetic implant oral rehabilitation were prospectively included in this study. For each patient three acquisitions EMG masseter and temporalis with a standardized protocol were performed. The determination of the VDO was obtained by modifying the provisional prosthesis with the aim of stabilizing the standardized indexes processed by the EMG apparatus software. The authors underlined that at the time of delivery of the final restoration, all sEMG standardized indexes showed values ??considered in the normal range. That instrumentally detect a perfectly integrated in the neuromuscular system occlusion and the individual correct VDO achievement. VDO occlusal adjustments are performed by evaluating the electrical muscle activity measured by EMG. The authors conclude that this procedure can positively affect the rehabilitation success rate because in neuromuscular balanced conditions overload components are reduced.
Quiet muscles for quiet teeth!
Link
The stomatognathic system abilities to adapt to the morphological changes are individual and variable. Clinical widespread opinion is that some patients “accept” morphological and functional changes related to dental work more easily than others. Most patients easily accept changes in shape, size and dental position; others are able to precisely detect changes, even limited to the tooth surface characteristics, less tolerating prosthesis not perfectly integrated in their oral biology. The adaptation ability is difficult to quantify, since there are no standardized and shared measurement parameters. Regardless of the patient we are treating, it seems still reasonable to limit as much as possible the required changes to its biology. Although it is a scientifically difficult demonstrable concept, we can suppose that an intervention which not affect muscle coordination is an intervention that probably will cause fewer technical complications. Indeed even the tooth not directly affected by rehabilitation procedures will benefit of bridges, crowns and implants that do not alter the chewing patterns; they will suffer the same initial stresses! Applying this concept in a prosthetic projection, we can mention the complication “fracture / chipping of an old reconstruction” immediately following the installation of a bridge, maybe the opposite side of the arch. Another clinical complication provides the appearance of pain in a tooth, following a occlusal change on the contralateral side of the mouth. In both cases, we could hypothesize that the intervention has caused a change in the oral proprioception, triggering a modification in muscles recruitment (then occlusal stress dissipation) that is the cause of the complication which occurred just a few hours away. Concept not widely recognized is that the dental occlusion is not a mechanical situation stable and constant. There are several demonstrations of how the “mechanical” relationship between the dental arches is susceptible to various conditions. For example, the study reported shows that the pain of the masticatory muscles can significantly alter the habitual occlusion (Effect of experimental jaw muscle pain on occlusal contacts. Mobilio N, Catapano S. J Oral Rehabil. 2011 Jun;38(6):404-9). In this dynamic view of dental arches relationship, it is more easily to understand the relation between changes in a dental area and any secondary complications in other areas of the mouth. Accounting that considerations, it seems reasonable to reduce unwanted muscular changes caused by dental treatments.
Reliable dental rehabilitation starts from dental occlusion managment.
Link
Restoration of patient dental occlusion, defined as osseous and dental static and dynamic relationships, may be needed for several reasons. Severe tooth wear, crowding, loss of masticatory units and oncologic surgical resections are the most common situations that require reconstruction of dental and/or skeletal occlusal relationships. Basically any dental work that changes the occlusal surfaces and/ or the tooth position could potentially modify oral proprioception. Kogawa., et al. [1] demonstrate how the interdental perception threshold in healthy subjects is less than 2 hundredths of a millimeter. It is very likely that dental treatments involving occlusal surfaces could change oral proprioception forcing neuromuscular patterns to develop functional adaptations. It has been clearly demonstrated how dental afferents play a role in the masticatory muscles recruitment. Occlusal modifications could change masticatory muscles global contraction intensity but also their functional relationship [2]. Indeed muscle imbalances may originate from several factors including a higher number of contacts, interference in the working or balancing side and loss of posterior vertical support [3]. Moreover, it has been demonstrated how proprioceptive dental alterations due to iatrogenic occlusal disturbances (200 µm thick) may require also neck muscles functional adaptations [4]. The role of occlusal-related functional abnormalities in the pathophysiology of Temporomandibular Disorders is still not clear; to date no scientific evidence-based conclusions are widely shared [5]. The relationship between abnormal muscle recruitment and symptoms such as pain or signs of dysfunction like movement limitation does not appear linear, underlining that a great number of subjects has a wide functional adaptability. The absence of clinical symptoms (mainly pain) following an occlusal intervention does not correspond directly to a procedure free from imperfections and/or anomalies. The muscles and nervous tissue adaptability to new oral conditions (without causing symptoms such as pain) [6] could “mask” changes in other structures, for example, teeth, bones and joints. Occlusal proprioception requiring (asymptomatic) muscle adaptations could causes changes in the distribution of the occlusal forces causing the following major complications:
In this context the use of masticatory function instrumental evaluations (before and after therapies that modify dental occlusion) are recommended to support the clinician to quantify the impact of occlusal changes on the oral biology. In fact, the biomechanical studies demonstrate that each muscle has its own specific action vectors (or more than one conferring redundancy features to the stomatognatic apparatus) and that alterations in the muscle forces distribution cause transformations of the mechanical stresses on the hard structures [7]. In conclusion, a reliable dental treatment must include a precise masticatory functional evaluation, not only to avoid the symptoms onset but also to ensure greater reliability and durability of homogeneously stressed oral rehabilitations.
Procedures to obtain an excellent masticatory muscles standardized surface electromyographic analysis.
Link
We desire to underline that video, edited by Prof. Claudia Dellavia from Università degli Studi di Milano. The video below shows the correct procedures to follow for an analysis of masticatory function with surface EMG. It gives reliable quantitative data even if made with standardized protocols that reduce biological and technical factors of variability. Among the different operative phases shot, a presentation of scientific articles that supports the illustrated sequences and for an in-depth analysis of anatomical and physiological concepts is shown.
The occlusal indicators may alter the performance of the masticatory muscles.
Link
The occlusal indicators are widespread in dental clinics to evaluate the distribution of the contacts between the dental arches. Often the distribution, number and highlighted contact area are used as an estimate of the “quality” of the occlusion itself. Researchers at the University of Loughborough (S. Forrester, RG, Presswood, AC Toy, MTG Pain) (UK) evaluated the performance of the masticatory muscles with and without occlusal indicators interposed between the arches. They have been assessed 4 types of occlusal indicators respectively of 24, 60, 96 and 202 µm thick. To numerically quantify muscle activation, Temporal and Masseter muscles electromyographic measurements were performed applying standardization procedures. sEMG standardized indexes have shown that exclusively indicators of 24 and 60 um thick did not cause significant changes in the masticatory muscles recruitment. The authors concluded as how occlusal indicators can alter the performance of the masticatory muscles then affect the measurement they provide (assuming the idea that muscle recruitment is one of the factors that determine the position of the jaw then so the occlusion. Editor’s notes).
Functionally inert occlusal protection-part IV.
Link
We want to end this 4-step videocourse “Functionally inert occlusal protection” with the splint adaptation to the modified oral conditions. Further dental reconstructions could modify the occlusal position and the splint has to be adjusted to the new anatomic situation.
Functionally inert occlusal protection-part III.
Link
After having created an occlusal splint planned for a simplified functionalization, we proceed to the splint installation on patient in respect of his dento-periodontal proprioception.
Functionally inert occlusal protection-part II.
Link
After having recorded the functional and morphological data, we purpose the second step of videocourse “Functionally inert occlusal protection”; the aim is to create an occlusal splint planned for a simplified functionalization.
Functionally inert occlusal protection-part I.
Link
We want to underline this 4 videos mini-course “Functionally inert occlusal protection” edited by Professor Dellavia. The aim of the cours is showing, in a simple and intuitive way, a dental treatment with occlusal protection splint in patients with an healthy stomatognathic apparatus; each operative section, regarding doctor and technician work, has been detailed in order to obtain a customized device that respect the patient clinical situation from the morphological and functional point of view.
Is an occlusal device enough?
Link
Interesting study published by André Luís Botelho, Bruno Caetano Silva, Flávio Henrique Umeda Gentil, Chiarella Sforza, Marco Antonio Moreira Rodrigues da Silva, Faculty of Odontology of Ribeirão Preto, University of São Paulo, Brazil. The Collegues analyse masticatory muscles function in TMD suffering patients with and without a resilient occlusal splint. Does a well designed and electromyographically functionalized oral appliance could improve gnatologic terapy outcome? It is enough to obtain symptoms relief?
Tonus or coordination?
Link
Interesting study published by Ellen Wen-Ching Ko et al., Department of Craniofacial Orthodontics of Chang Gung Memorial Hospital, Taipei, Taiwan. The Researchers explores the relationship between orthognathic surgery relapse and masticatory muscle activity investigated elaborating electromyography standardized indexes. Is muscular tonus more important than coordination in the treatment stability view?
Tooth displacement due to occlusal contacts.
Link
Tooth displacement due to occlusal contacts: a three-dimensional finite element study.Gomes de Oliveira S, Seraidarian PI, Landre J Jr, Oliveira DD, Cavalcanti BN. J Oral Rehabil. 2006 Dec;33(12):874-80.
Occlusal contacts in humans occur on inclined planes and have a great in?uence on maintaining tooth position and mandibular stability. When the occlusal system balance is disturbed some negative effects may take place. For example, muscular alterations, parafunctional habits, dental mobility, occlusal trauma, tooth migration and mandibular incisor crowding might occur. This last clinical condition is sometimes attributed to late mandibular growth, rebound of interdental ?bres or even to unerupted or erupting third molars.The use of the Finite Element Method (FE) is an appropriate way to study occlusal forces and tooth movement. The purpose of this study was to evaluate the effects of different occlusal contact patterns on tooth displacement in an adult dentition using a three-dimensional FE model of a human maxilla and mandible. Initially, images of a computerized tomography scan were redrawn in a computer program. Four occlusal patterns were tested:
FEM 1 – standard occlusal contacts;
FEM 2 – removal of mesial marginal and mesial tripoidism contacts;
FEM 3 – removal of distal marginal and distal tripoidism contacts;
FEM 4 – similar to FEM 3 with added contacts between upper and lower incisors.
The three-dimensional FEMs were submitted to static occlusal load tests to simulate the action of the muscles responsible for the mandibular elevation: masseter, temporal and lateral pterygoid muscles. These forces were applied at the FEM nodes representing the areas of anatomical insertion of theses muscles and the force vectors followed the muscle ?bers path. No muscular activity changes were simulated. FEM 4 data showed the largest degrees of displacements among all simulations tested. Despite having signi?cant lower incisor displacements, the results were even more remarkable when analysing the behaviour of the upper incisors antero-posteriorly. The only variable changed in this study was the point of force application by altering the occlusal contacts. Since these modi?cations simulated small clinical changes, the results may demonstrate the relevance of occlusal equilibrium on tooth position stability. In addition, the graphic representation of tooth displacements in all three planes of space presented in this study help to elucidate the effects of the resultant vectors caused by changing the dental contacts. Although the FEM loading was instantaneous (and dynamic stresses would undoubtedly be more complicated), the results of this study clearly showed that small alterations in occlusal contacts commonly observed in prosthetic, orthodontic or restorative treatments could disrupt the balance of the occlusal system.
Standardized electromyography, why?
Link
Dental therapy often modified the patients occlusion, understood as the bones and dental relationship, static and dynamic. Severe tooth wear, crowding, loss of masticatory units and surgical resections due to neoplasms, are the main situations that require occlusion and dental reconstruction. Basically any dental work that changes the occlusal surfaces and/or the position of the teeth can potentially alter proprioception; Kogawa et al. (J Oral Rehabil. 2010; 37: 322-8) show that the perception threshold can reach the 2 hundredths of a millimeter. Frequently the dental procedures cause changes in proprioception oral forcing the neuromuscular system to implement functional adaptations. It has been clearly demonstrated as dental afferents play a role in the recruitment of the masticatory muscles. Dental occlusion changes can vary the intensity of the global contraction of the different masticatory muscles but also their relationship (Wang et al. Acta Odontol Scand. 2009; 67: 187-192). Muscle imbalances may originate from a number of factors such as inconsistencies between the occlusal surfaces, interference in the balancing or working sides and loss of posterior support (Trovato et al. Stomatologija. 2009; 11: 26-31) (in addition to pain stimuli caused by inflammatory or degenerative phenomena that should be excluded before performing a functional assessment). It was also demonstrated as proprioceptive dental alterations due to iatrogenic occlusal disturbances (200 µm thick) may require functional adaptations also to the muscles of the neck (Ferrario et al. J Oral Rehabil. 2003; 30: 34-40). Electromyography standardized can be a useful aid in the instrumental evaluation of dental proprioceptive related muscle adaptations and can providing guidance to the clinician to reduce the complications of reconstructive therapies.
The new easymyo website is now available!
Link
Scientifical, clinical and commercial info to an efficient everyday use. Continuous updates about standardized electromyography on our blog and Facebook profile.